WHEN’S THE LAST time you were in a hospital? As the patient.
Maybe it’s been a while. Here’s how it goes, usually: You’re in the bed. Seven a.m. is shift change. The night nurse comes in—she’s going home, so she makes sure everything is all set for the day nurse. (You think you know what nurses do, but until you spend some time in a hospital, you have no idea. Nurses run health care.)
Guy shuffles in to take the trash. He whips the new bag in the air, and the noise is like a firecracker.
Does he not know I’m sleeping?
You didn’t sleep much, what with the beeping machines, the whirring of the IV, the glow of the monitor logging your pulse, blood-oxygen level, everything.
A woman comes in to wipe everything down. The bracing smell of the disinfectant cools your nostrils. There’s something comforting about it—everything is clean now.
Soon the doctor will burst in, a phalanx of residents and fellows trailing her.
You’ll rub your eyes.
Is breakfast here? I ordered it last night, on the little sheet, like they said.
They’ll read off your medical history and the last time you had a bowel movement. The doctor will speak loudly, and you’ll wonder why so loud.
So many people, you’ll think.
When you’re in the hospital, all you think about is leaving. You’re sick or you’re hurt, and you’re not thinking about who these people are. They aren’t people with families and back pain and a bag lunch in the fridge down the hall.
And that’s okay. Nobody works in a hospital for the glory. Their calling in life, if you think about it, is to get you out of the hospital.
But now? Amid a pandemic? This is when we’re reminded that in this work, these people are heroes. They have always been heroes, just as firefighters were heroes long before 9/11.
We just didn’t know it.
A hero, we are reminded by all of this, is someone who puts himself or herself in harm’s way to help another person. Here is what harm’s way means right now: The Centers for Disease Control reported days after these photos were taken that between 10 and 20 percent of all confirmed COVID-19 cases in the United States were likely health-care workers, and 27 had died.
On April 9 and 10, when the COVID crisis was at its height in New York City—when New York City was once again ground zero of a vicious attack—we sent a quarantined photographer, Benedict Evans, and his assistant, Marion Grand, to two of the biggest, most central hospitals in Manhattan: Weill Cornell Medical Center on East 68th Street, and Columbia Presbyterian, at 168th Street and Broadway. He stationed himself wherever it was safe to set up his simple apparatus, and we worked with the hospitals to make sure his work would not impede the administering of care.
In those two days, he photographed 17 remarkable people.
Oh, they’re not heroes—that’s what they’ll tell you. Just doing their jobs. Well, we’re all just doing our jobs. But for most of us, no one is dying in our hallway, no grandmother is wheezing in our arms, no father is begging us to let him touch the glass that separates him from his daughter, one last time, before the end he knows is coming.
With any luck, you won’t be in a hospital any time soon. But if you are, try not to get annoyed by the guy taking out the trash. Or the nurse who let the door close a little too loudly.
They’re just doing their jobs.
Photographs and Interviews by Benedict Evans
JOSEPH GALIZIA
30, critical-care paramedic, NewYork-Presbyterian
MY POSITION IN the hospital allows me to see a lot of high points, because I see things from street level all the way up to the ICUs. And the high point is that everyone’s working together to beat this. Every time I come into work, that’s a high point, because we’re all still showing up. Paramedics, EMTs, doctors, nurses, patients, support staff—everyone is showing up to work still. And that’s a high point.
While I’m at home, I’m trying to make things feel as normal as they can. You know, eating on a normal schedule, working out on a normal schedule, studying as much as I would normally do. I feel like the best thing we can do is try to maintain a sense of normalcy as much as we can, so we can stave off any feelings of anxiety. Because—things are different now, but they don’t have to be that different while we’re at home.
CARA AGERSTRAND, M.D.
40, pulmonologist and intensivist, NewYork-Presbyterian/Columbia University Irving Medical Center
ON THE DAY we got our first COVID-positive patient here in New York, I was in a medical conference with several other colleagues in my specialty, and within what seemed like minutes all of our phones started going off, we started getting texts and calls just left and right. And it made everything really hit home that this is something that could be really impactful here. Not just in Italy, not just in China.
When I come into work in the morning is probably the most difficult part of the day. Because I ride a bike, and I look down these empty streets of New York that are normally bustling with people and cars and traffic, and they’re deserted. And yesterday I was riding in listening to “Mad World,” thinking, How have we found ourselves in this situation? The streets are so empty, but the hospital is so full of so many sick people.
JAMES ZABALA, R.N.
37, staff nurse, NewYork-Presbyterian/Weill Cornell Medical Center
FOR THE MOST part, we don’t allow visitors to the hospital. So some of our patients—even though we try to do as much as we can to connect them with family with FaceTime or conversation on the phone, oftentimes they’re in the room by themselves. That’s kind of a low point. I mean, they’re not alone. We’re there. The nurses are there. The doctors are there to support them in their last moments, when they breathe their last breath. But those have been the low points for me. Usually they’re surrounded by family. It’s a little harder here when you’re the family for them.
There’s this one physical therapist at work that has like this mindfulness thing he does with all of us. Kind of like: Take yourself out for a moment, pause, focus on your breathing. I modify it to me. I really like music. So I’ll turn on my favorite track for the day, and I focus on one specific thing, like a treble or a bass—I focus on that rhythm, like, boom, boom, boom. I tune everything else out. Like the lyrics—all the rest of the song. And it kind of takes me out for however long—a minute or two—out of my situation. I take my 30 seconds or 20 seconds or a minute to myself, and that usually does my mind a lot of good.
MARIE-LAURE ROMNEY, M.D.
40, emergency-medicine physician, NewYork-Presbyterian/Columbia University Irving Medical Center
THE GRAVITY OF the situation really hit me when I went to one of our hospitals, one of the EDs [emergency departments], and it was unrecognizable. It felt like I’d walked into an intensive-care unit and not the ED that I’d been working in for the last 18 months. I think I was mostly struck by how sick all the patients were, but also by the fact that they were all by themselves without family there. It was a really challenging moment, a very somber moment.
We talk about the silver linings in this entire crisis. The time that I’m getting to spend with my children and my husband, who otherwise would have such full schedules that we don’t often overlap, but they’re reliably home when I get home from work—it allows me to kind of escape and pause from thinking about all the terrible things that we’re seeing at work. I find that to be really rejuvenating.
WALLACE CARTER, M.D.
64, emergency-medicine physician, NewYork-Presbyterian & Weill Cornell Medicine
ONCE WE STARTED seeing the reports from the West Coast, and we started to take stock of where we were here at NYP and what we were going to have to do to prepare for it, it became brutally real and incredibly…I think that’s when we all realized that we could potentially be in for something that we had never seen before.
I signed up for this. This is what I love to do. I was one of the earliest paramedics in New York City in 1977, and I’ve been through just about every disaster in New York City: both of the World Trade Center events, plane crashes, the HIV/AIDS epidemic back in the ’80s. What gets me, what inspires me, is to come to work every day and realize that we can make a difference and that my being here is important to the institution, to the patients, to our colleagues, to the residents. I’m making a difference. That’s what inspires me.
EUGENIO MESA
28, environmental-services worker, NewYork-Presbyterian Morgan Stanley Children’s Hospital
MY SUPERVISOR CALLED me to the side and asked me if I have a problem going into these rooms. I said, “No, I have no problem. As long as I have the proper PPEs and the proper equipment to go into rooms, I wouldn’t mind to go in.” If that was me in that bed, I would like people to come inside and, you know, clean for me. Because that’s what we’re here to do. Making sure everything is clean and organized so the doctors and the nurses can do their job. So she just asked me, Can you go inside this room? I say, “Of course I can.” That’s how everything started. Ever since that morning, we just work without stopping.
AYA ISLAMOVA, R.N.
35, clinical nurse, NewYork-Presbyterian/Columbia University Irving Medical Center
WE KNEW THAT it was coming, but we are not prepared for that moment. I was at work that day and we got an emergency meeting with our manager. We stopped what we were doing and it’s announced that our unit will become a COVID-positive unit. It was a very frightening moment. It was a feeling that I want to leave the place and I want to go home to my loved ones. But obviously you can’t, because you have patients to take care of, you have five, six patients at a time.
We’ve been taught about our self-care, which means stay healthy. Not only physically—mentally, spiritually. You try to take those short breaks, leave the floor, hydrate yourself, eat well. But in real life, sometimes it’s not happening because you’re so busy, and you realize that it’s 5:00 p.m. and you haven’t had your break. You haven’t gone to the bathroom.
GREGG ROSNER, M.D.
40, cardiologist and cardiac intensivist, NewYork-Presbyterian/Columbia University Irving Medical Center
I THINK AFTER that first week, I became numb. In order to do this job, you have to be able, in some ways, to separate out the suffering of the patients, the families, in order to continue to do your job. I tend to be mission oriented. And the mission is: Come in, take care of patients, do everything you can to make them better. I try not to think much more than that.
I’ve never heard the word no in the past four weeks, and that’s not typical for a large institution. Everyone just takes the mission seriously. And to me, you sort of see the best in humanity during these crises. We’re socially distancing, but in many ways—I know more nurses’ names now; the nurses are being floated in and out of units that they never work on; I work with other doctors and other fields closer than we had ever worked before. And so, in many ways, I feel more connected to people at work rather than less connected.
KENNETH MALLEY-FARRELL, R.N.
46, neuro-intensive-care-unit nurse, NewYork-Presbyterian/Weill Cornell Medical Center
YESTERDAY AND THE day before and the day before and the day before—they all kind of just melt into one at this point. This is my 28th day in a row. Each day you come in and it’s just a new crisis. Or it’s almost always a new crisis. We just try to deal with them as quickly and as professionally as we can. I think, coming into work, I’m always hoping for that patient to get extubated today. Or that patient, their labs to just look a little bit better today. And it’s very slow. It’s not like anything we’ve ever seen. These patients, they stay sick for so much longer than what we’re used to. So each day the hope is that there’s gonna be an improvement.
I used to get frustrated with my father, who died 16 years ago, because he always did above and beyond for people, and he didn’t get the gratitude he deserved. And he did it for people who just didn’t deserve it sometimes. And I asked him why he did it. And his answer was always the same. It was: “Because you should.” And that’s what keeps me going.
TRUDI CLOYD, M.D.
35, emergency-medicine physician, NewYork-Presbyterian/Columbia University Irving Medical Center
I ACTUALLY WAS one of the people that got confirmed as testing positive, and I had about 12 days at home quite sick. I’ve made it through and now I’m back to work. I’ve been pretty eager to get back in there. But a lot changed in those 12 days. I went back, and I walked around and every single person in every room was on a vent or on a non-rebreather, and it was so eerie. It was like I was in some alternate universe. On a normal 12-hour shift, we might have one or two of those patients come through the emergency department. And for it to be every single patient, sometimes even two a room, it was like: What happened? In 12 days, the world had turned upside down.
Being somebody that’s recovered from this illness myself, I’ve really enjoyed having the chance to talk to the patients about their symptoms and what they’re going through, because I feel like I can really identify with what they’re experiencing. It was a very scary experience for me as well. You cannot breathe. You are very light-headed. You feel like you’re gonna pass out. You have fevers that don’t go away for days. I understand what they’re going through. I understand why they’re scared. And I’m trying to reassure them, because if their oxygen saturation is fine, then they’re okay and they don’t need to be admitted. But that doesn’t minimize the symptoms and the fear that they’re experiencing.
I’m from the South originally. So I feel like I have different standards for general kindness and friendliness on the street than what New York City normally is. But I got so many notes under my door from neighbors! I got people asking what prescriptions they could go pick up for me. I had people getting groceries. I had colleagues come by and demand to take my laundry, because I couldn’t do my laundry for two weeks. And it was just—it was amazing. It was the type of thing where New York comes up and totally surprises you. Because when real challenges come, then people really come together.
ALEXANDER FORTENKO, M.D., M.P.H.
33, emergency-medicine physician, NewYork-Presbyterian & Weill Cornell Medicine
WE’D BEEN GEARING up for this for maybe a month before things really hit. But I remember about three weeks ago, working an overnight—I came in, there was chaos in the bay, multiple critically ill patients all at once, really for the first time at our hospital during this pandemic. And we knew that there was something different about that night. We knew that things had changed, things had shifted. I remember walking out of the hospital and actually calling my wife in the morning after my shift was over. I remember getting on the phone with her and I said, “I think it’s here now.”
As emergency-medicine doctors, you know, I’m on the front lines, but we also have to think about all the other people that take care of these patients. So the nurses, the PAs, the nurse practitioners, the techs, the janitors that go in and clean the rooms afterwards. I was fairly certain that they were spending more time with these patients and in the rooms than I was, putting IVs in, comforting the patients, making sure they were sedated if they were on a ventilator. And so I feared for them. I didn’t really fear so much for myself. But I have an eerie feeling every time I go to work. I used to really, really love my job, and I still love my job now, but I now sense something that I never really sensed before, which is a sense of worry and fear when I go to work.
RAHUL SHARMA, M.D.
45, emergency physician-in-chief, NewYork-Presbyterian & Weill Cornell Medicine
YESTERDAY, WHAT WAS on my mind is how are we going to deal with tomorrow? What are we going to do differently? How are we going to prepare? Constantly watching the news to see where the numbers are. When are we going to plateau? What are the number of deaths gonna be tomorrow versus today? That’s what’s been going on day by day: How many patients are going to require ventilators? How are we doing overall, not only in New York but throughout the country?
What inspires me is being in the specialty of emergency medicine. We went into this specialty to deal with disasters, to deal with chaos, to deal with these kind of pandemics. But this is real life now. It’s inspiring to see all the front-line staff, how they’ve come together, the camaraderie that I’ve seen. Clapping every night in New York City at 7:00 p.m., that’s inspiring. The food and the donations that we’ve had from everyone, the generosity—all of that has been inspiring and actually gets me through the day.
DIANA BRICKMAN, R.N
32, critical-care nurse, NewYork-Presbyterian/Weill Cornell Medical Center
WHAT WAS ON my mind yesterday when I was on my way to work was fear. It was one of the first times I’ve been back to the bedside in two and a half years. I’m in an education role now, so I was afraid that I’d lost my skill. Luckily, I didn’t, but there was fear. And there was fear of catching it. You know, I’m worried about myself. I’m worrying about bringing it home to my family. But there’s also confidence, and as soon as I walked in here, I knew I had a job to do and the patients were relying on me to care for them, and although I wasn’t in the COVID unit, I was with the other patients who are even more scared and going through surgery, and I had to be there for them. So I became confident.
ANDREW AMARANTO, M.D.
42, emergency-medicine physician, NewYork-Presbyterian Lawrence Hospital
I REMEMBER DISTINCTLY, I was driving to work from New Jersey, crossing the George Washington Bridge. It was March 1, and I got a call from infectious disease at the hospital that we had cases of what we’re calling “community acquired COVID,” meaning these are not travelers, these were folks from the community. I have this vision of driving across the George Washington Bridge and glancing down at Manhattan and thinking about what that would mean to have community-acquired disease in a congested city like New York, and literally from that day forward, life hasn’t been the same.
It’s an interesting situation for us, with my wife being sick and the amount of exposure that I have. Our six-year-old is staying with my in-laws, and I see him when we go on a walk or two a day. He’ll come out of the house and—we maintain distance—he brings the dog and we go on these long walks. Sometimes we’re going at night after I come home, it’s late—and my son invented shadow hugs, where we stand so that the streetlights hit us just right, we get our shadows to hug and give high fives. Those are the best five minutes of my day.
CARLOS POLANIA
29, respiratory therapist, NewYork-Presbyterian/Weill Cornell Medical Center
I HOPE THAT people will learn to take better care of themselves. You know, this COVID virus is affecting a lot of different people, even people with no known past medical histories or present comorbidities. But people who do have past medical histories—hypertension, diabetes, smokers—they’re really being affected by it, some severely, even to the point of death. So I just hope that after all this is over, people learn to take better care of themselves. Stay healthy, work out, eat well, and just appreciate and take care of their bodies. Because we only get one life, one body, and if we don’t take care of it, and something like this ever happens again, a lot more people aren’t gonna make it.
CHRIS REISIG, M.D.
38, emergency-medicine chief resident, NewYork-Presbyterian/Columbia University Irving Medical Center & Weill Cornell Medical Center
I’M A LITTLE anxious when I’m heading in to work. You know, I think your nerves get to you when you’re not doing something. But I found that, for the most part, when I get to work—it’s a familiar place, it’s a place I’ve been for years at this point, it’s the people I know, it’s the same things that I’ve done every day before this. And so the longer I manage the shift, the more relaxed I tend to be, just because it’s familiar. But that clock kind of resets every day, too.
Work is usually pretty much nonstop. You kind of take a deep breath at the start of 12 hours and you exhale 12 hours later. Outside of work, I’m very lucky to have a family who has stayed with me in the city. So my life outside of work is where I recharge as much as possible just being with my wife and my kids. But each shift is 12 hours of pretty much nonstop.
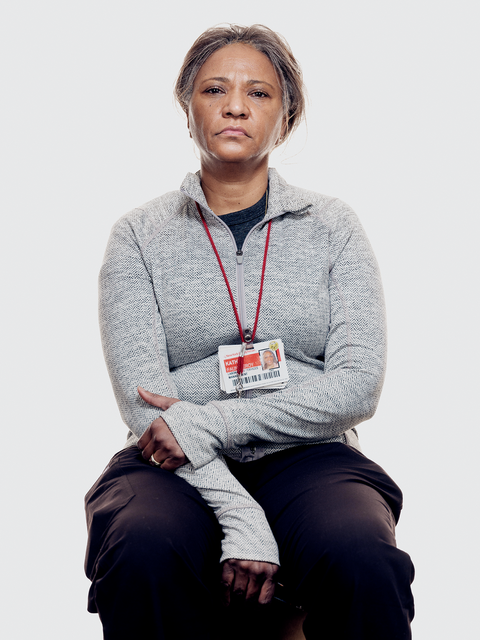
KATHY FAUNTLEROY
58, microbiology-laboratory supervisor, NewYork-Presbyterian/Weill Cornell Medical Center
THIS IS WHAT I was trained to do. I’ve spent more than 30 years doing this job. And you learn in school and you learn in safety training that you have to be ready for an event like this. And you always have it in the back of your mind, but you never really think that it’s actually going to happen. But when it does, you go right to the training that you had. So I feel good that I was trained properly and that I was able to bring my best to this situation.
I have moments where I duck into a bathroom to pray. Sometimes.
BEHIND THE SCENES WITH PHOTOGRAPHER BENEDICT EVANS
EVERYTHING HAPPENED VERY quickly. I got the call three days before we started shooting, and in that time I went on two different scouting trips to find areas around the hospital that were safe yet not in the way. We had a crew of one—it was me and my assistant. The night before we started shooting, my heart was beating quite quickly. Once we got into it, though, it was probably less risky than going grocery shopping in New York at the moment. The last thing these people want is another patient in the hospital, so they take protection very seriously.
Being among these folks was emotional. Many of them had just come off long shifts—a couple of them looked like they were about to keel over in front of me. But we didn’t want to sugarcoat it. We wanted to show them as they looked and felt.
What I hope people take away from this portfolio is that these health-care workers are heroes, but they’re also normal people. They don’t have superpowers to enable them to get on with this. It’s why I photographed everybody with their masks and PPE on and off. On one hand, when you cover up someone’s face, you lose some of their humanity. But on the other, I can’t imagine the horror of those dying from COVID-19—whose only human contact in their last days and hours is with people whose faces are covered.